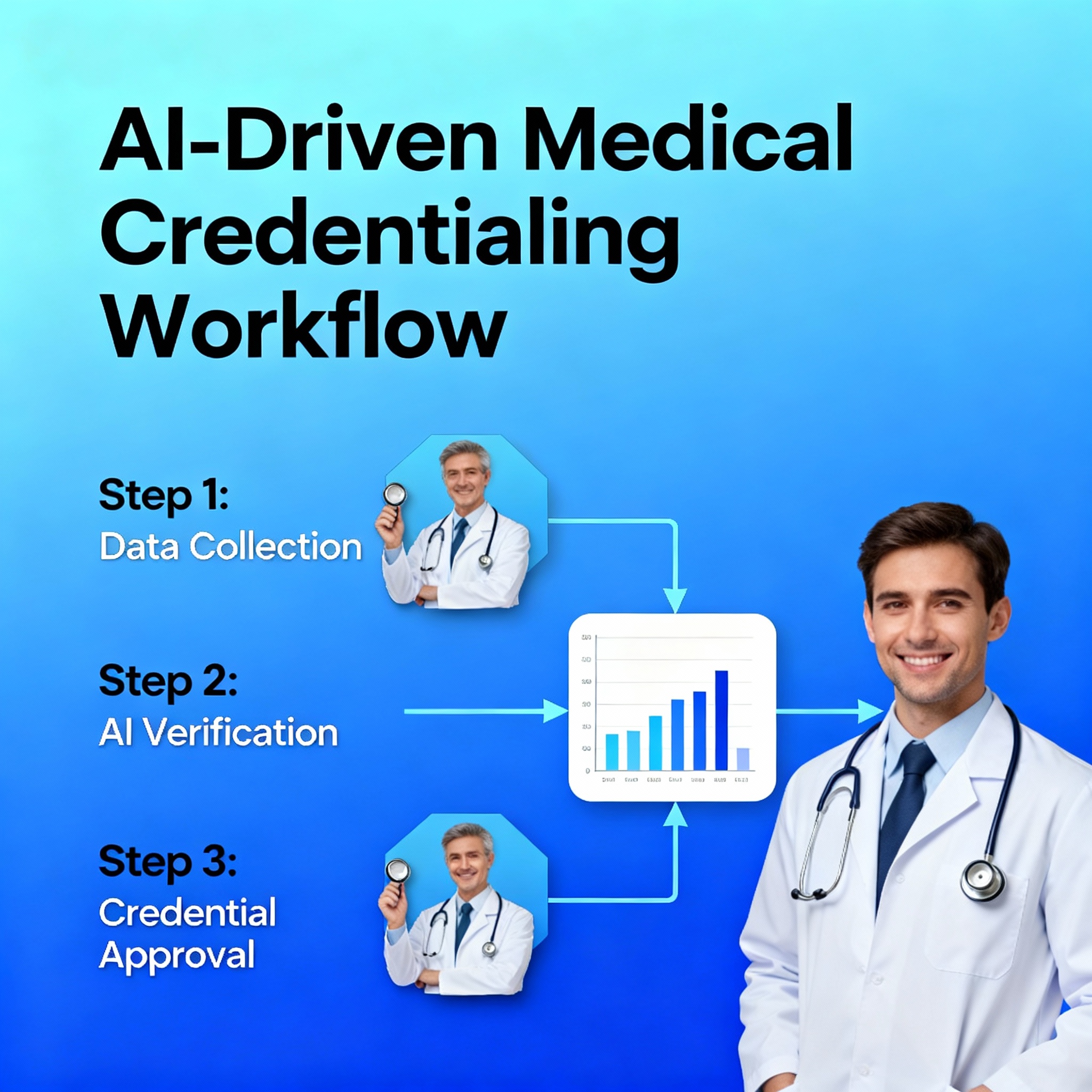
Powered Medical Credentialing Revolution
Transform your credentialing workflow with advanced technology. Reduce processing time by 60% while maintaining 99.8% accuracy through intelligent automation.
Learn More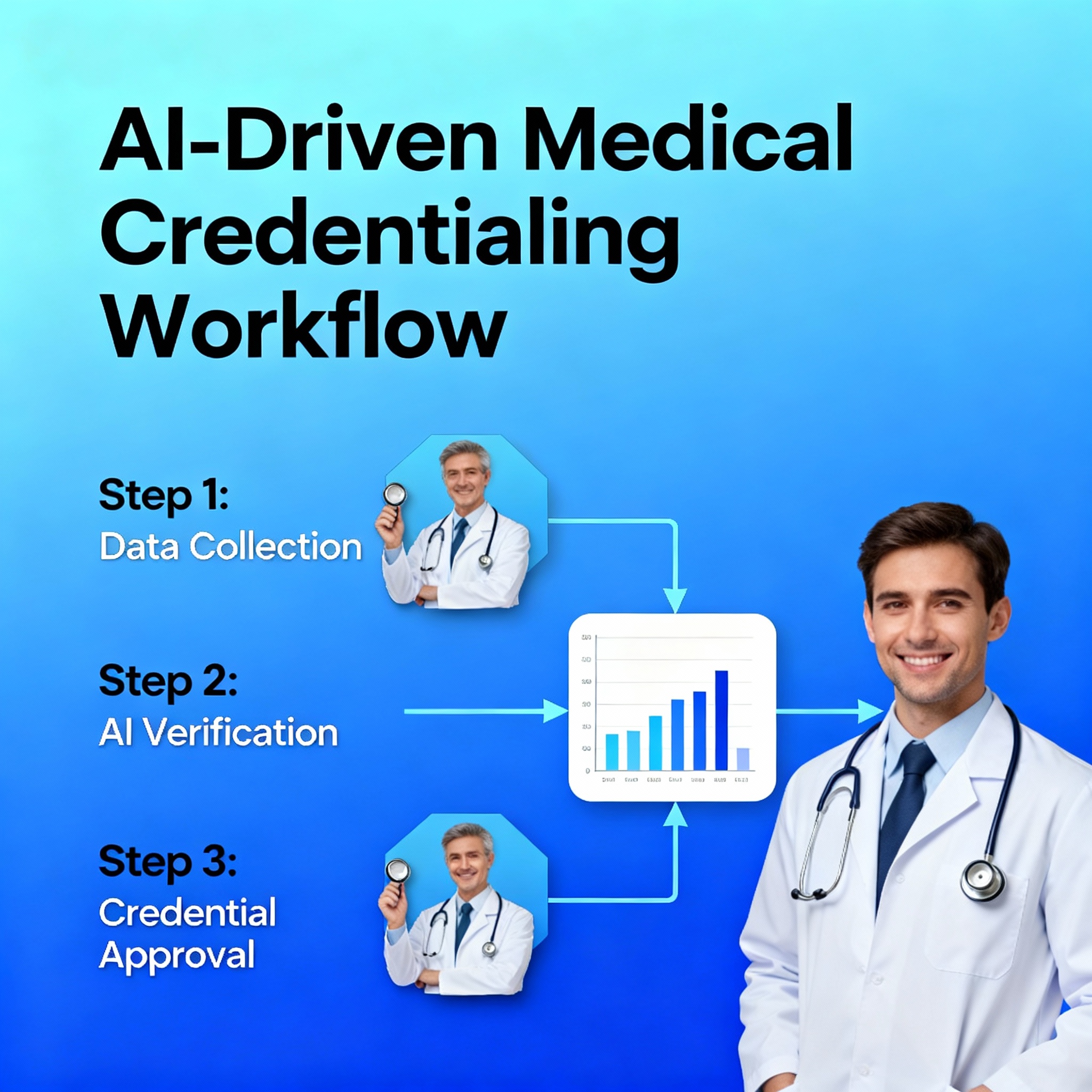
Real-Time Verification System
Instant verification with licensing boards, medical schools, and government databases. Ensure authentic credentials with real-time data validation.
Learn More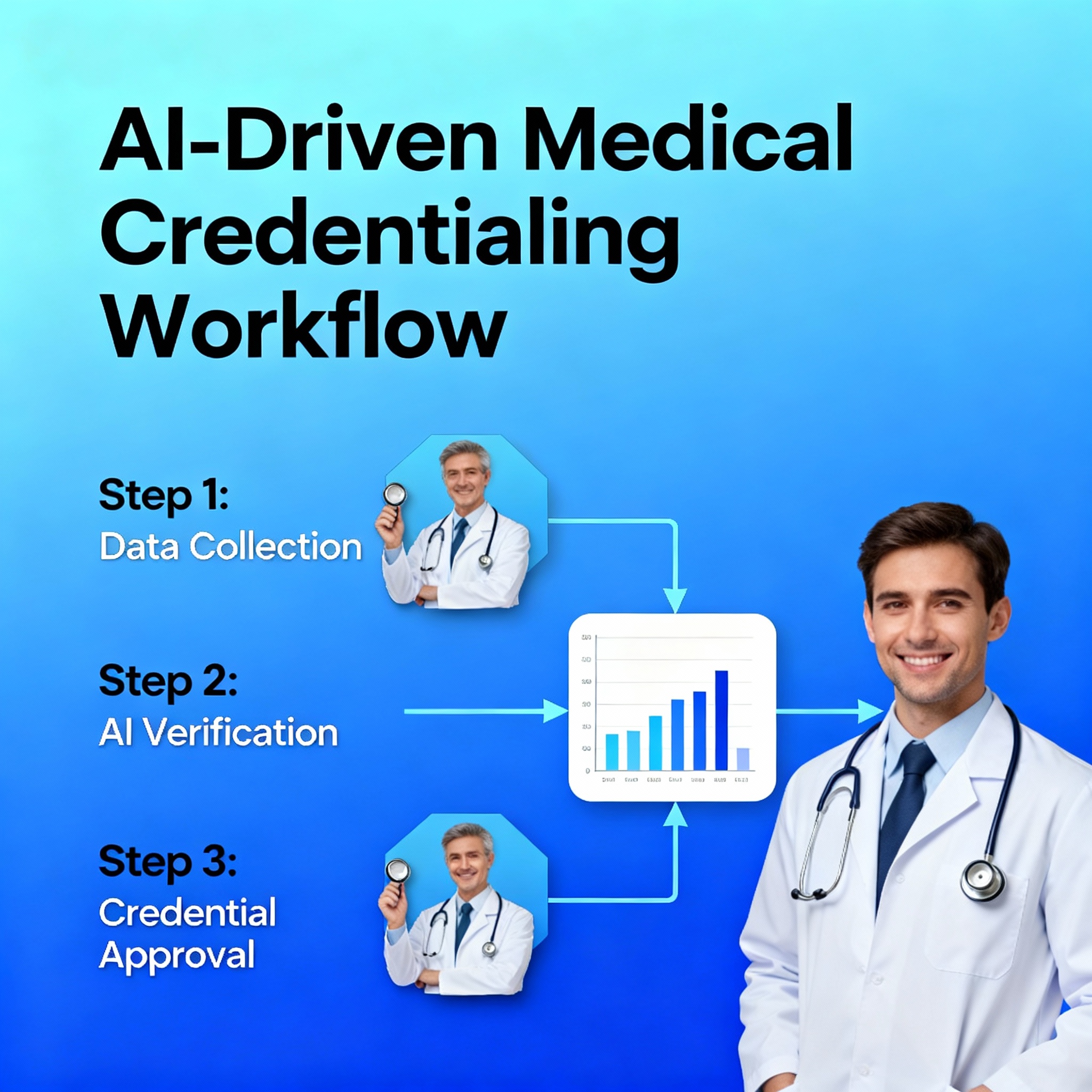
Automated Compliance Monitoring
24/7 continuous monitoring for license expirations, sanctions, and regulatory changes. Receive instant alerts to maintain complete compliance.
Learn More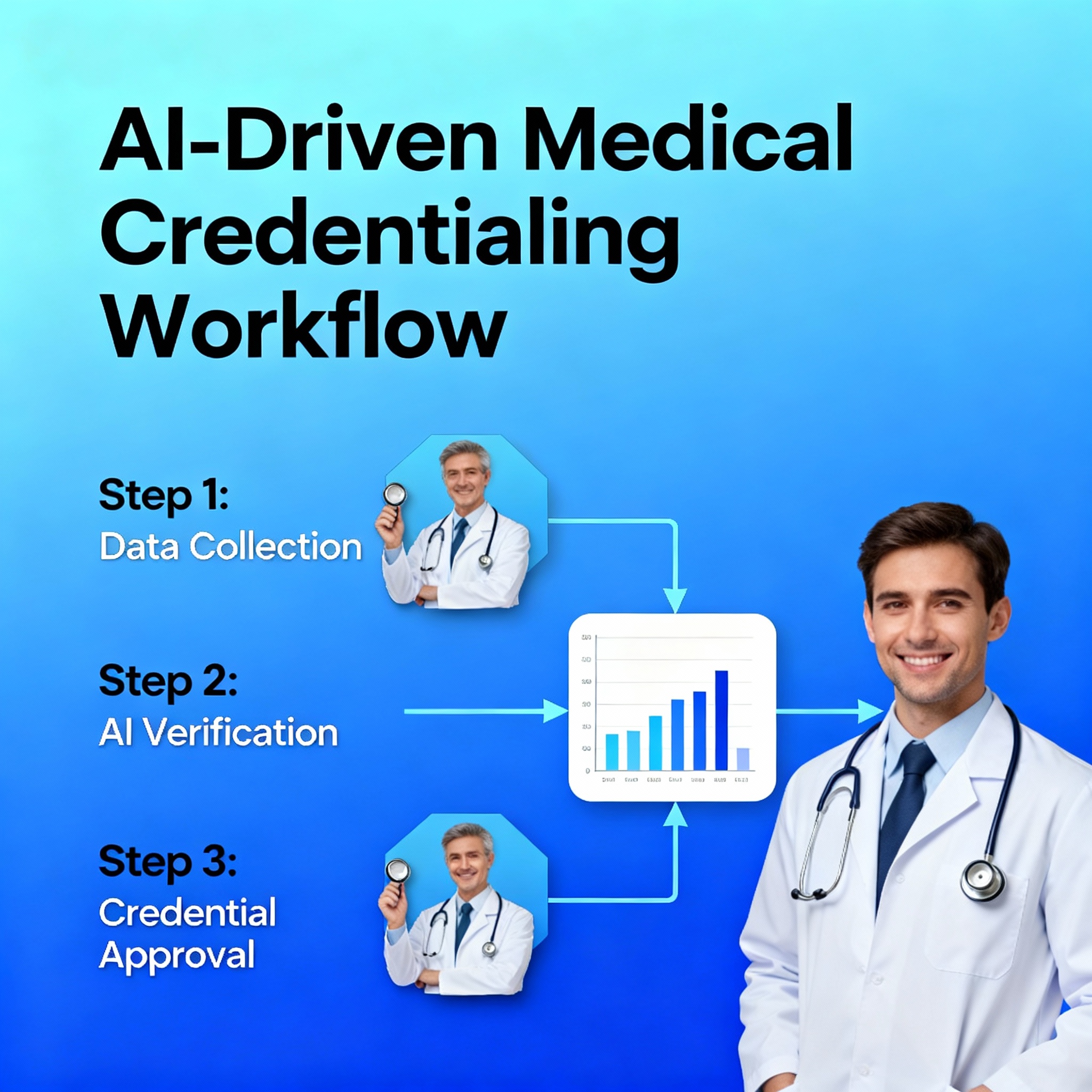
Comprehensive Analytics Dashboard
Real-time analytics and custom reports provide full visibility into your credentialing pipeline. Track performance metrics and optimize workflows.
Learn More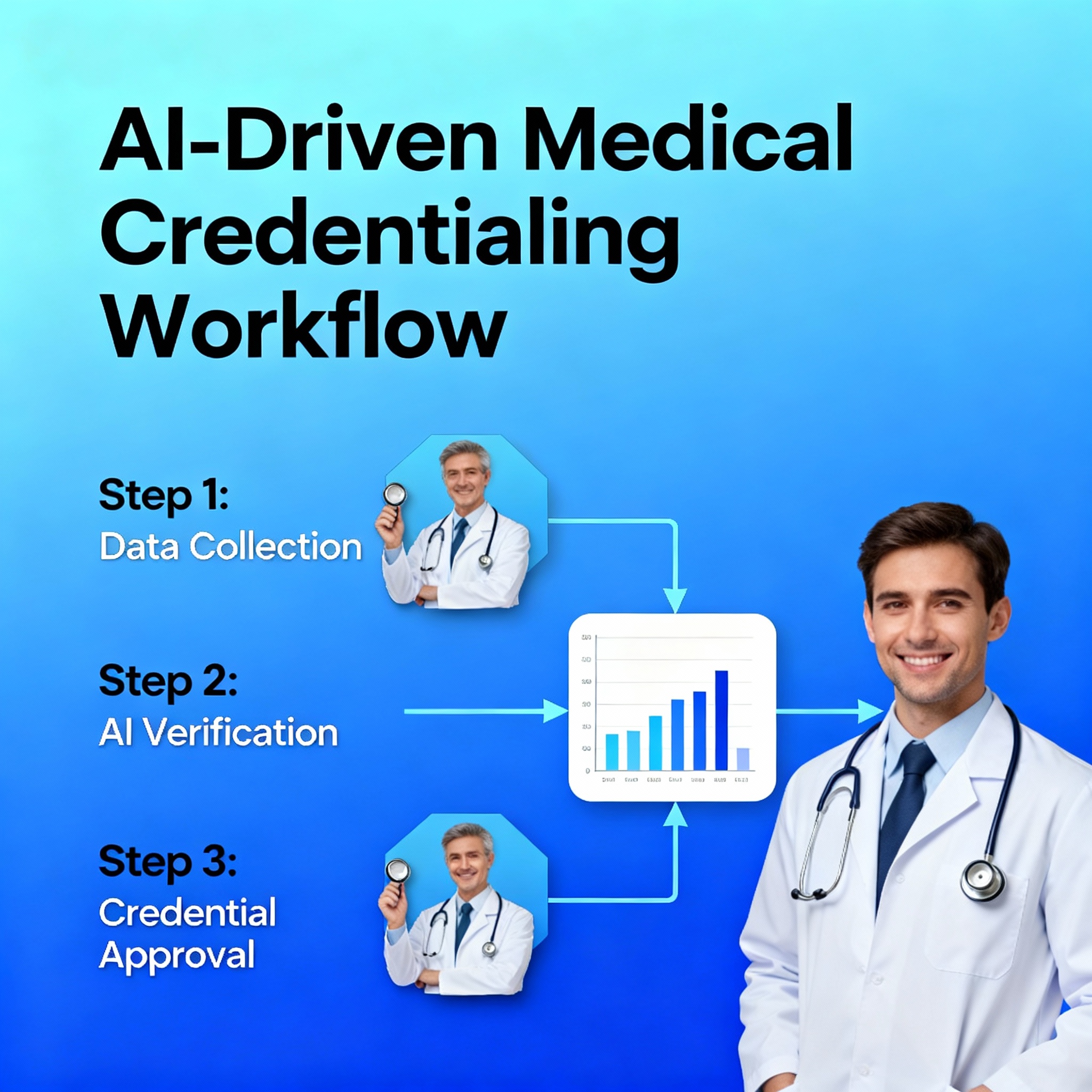
Streamlined Provider Enrollment
Complete credentialing packages ready for provider enrollment. Seamless integration with CAQH ProView and payer systems.
Learn More